What’s worse than a migraine? 5 things to know about cluster headache
August 13, 2018
(BPT) – Cluster headache (CH) is an extremely painful primary headache disorder, which affects one to two people in every 1,000.[1] CH is known as being one of the worst pains known to man and is even more debilitating than migraine. Listed below are five important things to know about this condition.
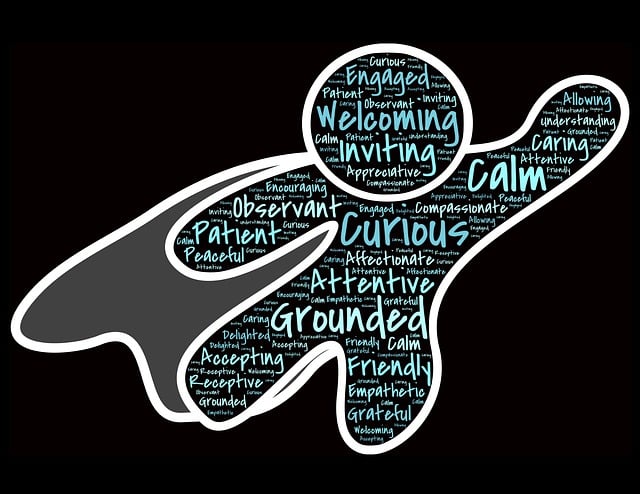
1. Recognize signs and symptoms

The most common sign is sharp, excruciating pain, usually centered at the eye, temple, or forehead that attacks one side of the head.[1] CH typically occurs in bouts (or “clusters”) for 6 to 12 weeks, often at the same time each year or day.[2] Each bout lasts from 15 minutes to several hours, and can strike up to 8 times a day.[3]
2. Determine risk factors

Pay extra attention if you’re a male, smoker or have a family history of CH. It predominantly occurs in males, with symptoms typically manifesting by the age of 30. Those at greater risk of CH include heavy smokers and individuals with a family history of the condition.[4]
3. Speak to a doctor

CH is nicknamed “suicide headache” as patients diagnosed with CH take their lives twenty times more often than the national average due to the excruciating pain.[5] If you or someone you care about is suffering from any or all of these symptoms, it is important to speak with a physician, such as a neurologist or headache specialist.
4. Develop a treatment plan

There are treatment options for CH. A physician can help develop a treatment plan to manage CH. Historically, prevention and treatment strategies have been a challenge, but advances in the area — including new technologies — are offering patients innovative, non-invasive solutions.
5. Explore novel non-drug treatment options

gammaCore®(nVNS) is the first non-invasive vagus nerve stimulation therapy applied at the neck for the acute treatment of pain associated with episodic CH and migraine in adult patients. For more information, visit http://gammacore.com/.
Important Safety Information regarding gammaCore
gammaCore (non-invasive vagus nerve stimulator) is indicated for the acute treatment of pain associated with episodic cluster headache and migraine in adult patients.
- The safety and effectiveness of the gammaCore non-invasive vagus nerve stimulator (nVNS) has not been established in the acute treatment of chronic cluster headache.
- gammaCore has not been shown to be effective for the prophylactic treatment of migraine headache, chronic cluster headache, or episodic cluster headache.
- The long-term effects of the chronic use of the device have not been evaluated.
- Safety and efficacy of gammaCore has not been evaluated in the following patients, and therefore is NOT indicated for:
- Patients with an active implantable medical device, such as a pacemaker, hearing aid implant, or any implanted electronic device
- Patients diagnosed with narrowing of the arteries (carotid atherosclerosis)
- Patients who have had surgery to cut the vagus nerve in the neck (cervical vagotomy)
- Pediatric patients
- Pregnant women
- Patients with clinically significant hypertension, hypotension, bradycardia, or tachycardia
- Patients should not use gammaCore if they:
- Have a metallic device such as a stent, bone plate, or bone screw implanted at or near their neck
- Are using another device at the same time (e.g., TENS Unit, muscle stimulator) or any portable electronic device (e.g., mobile phone)
Note: This list is not all inclusive. Please refer to the gammaCore Instructions for Use for all of the important warnings and precautions before using or prescribing this product.
gammaCore is available by prescription only. U.S. Federal Law restricts this device to sale by or on the order of a licensed healthcare provider.
[1] Rossi P, et al. Funct Neurol. 2016;31(3):181-183.
[2] Cluster Headache. American Migraine Foundation. https://americanmigrainefoundation.org/understanding-migraine/cluster-headache/. Accessed January 3, 2018.
[3] Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33:629-808.
[4] Cluster headache. The Migraine Trust. https://www.migrainetrust.org/about-migraine/types-of-migraine/other-headache-disorders/cluster-headache/. Accessed January 5, 2018.
[5] Fletcher J (2015) Why Cluster Headaches Are Called “Suicide Headaches”. J Neurol Stroke 3(3): 00092. DOI: 10.15406/jnsk.2015.02.00092.